Providing the highest standard of care for ADHD patients is at the core of clinicians’ goals. However, without the right metrics in place, clinicians cannot systematically track performance from patient to patient, across clinic sites, and over time. Developing a consistent set of quality indicators for ADHD care is therefore essential to drive improvements that will benefit patients and clinicians.
“Standardized measures that allow results to be monitored and tracked uniformly over time are the foundation of performance improvement.”
- Kilbourne et al.
Challenges and Opportunities in Measuring the Quality of Mental Health Care
What metrics should ADHD clinicians be tracking in 2025?
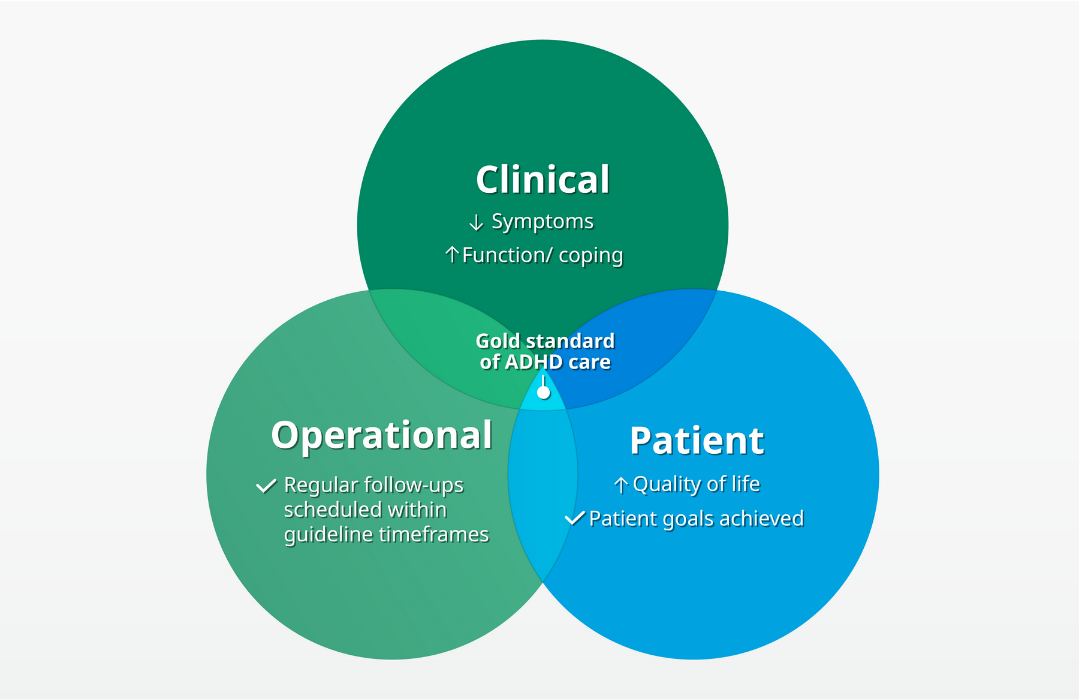
There are three core areas for ADHD success metrics: clinical outcomes, operational outcomes, and patient-centered outcomes. Consistently meeting goals across these areas will lead to continuous improvement and better care outcomes.
1. Clinical outcome metrics
Quantifying symptom change after starting a new ADHD treatment is an important part of the titration process to find the right care plan for the patient. Tracking symptom reduction also serves an independent function as a performance improvement metric.
In the US, the AAP recommends using “DSM-5 based ADHD rating scales” for diagnosis and tracking symptom change. As an example, there are specific follow-up (post-treatment) Vanderbilt scales for parents and teachers to assess symptom change in children with ADHD.
In the UK, in addition to these subjective rating scales, an objective test is recommended by NICE as part of the ADHD diagnosis process for children and young people aged 6-17.
Using an objective test to quantify symptom change in ADHD patients
A digital ADHD technology like QbCheck provides clinicians with objective data on a patient. Results can be compared over time to monitor symptom change post-treatment and provide valuable metrics to help quantify improvements.
The Founder and Mental Health Nurse Practitioner at Focus of Tampa Bay shared her positive experience of using an objective test:
“Adding objective data to our ADHD diagnosis process helps us find the missing pieces, enhancing patient care.”
- April Green, APRN, FNP-BC, PMHNP-BC
2. Operational outcomes
Clinicians should also track the timeliness and effectiveness of patient care delivery.
The National Committee for Quality Assurance (NCQA) standard for ADHD care tracks the percentage of children who have at least three follow-up visits within 10 months, including one within 30 days after their first ADHD medication is prescribed.
Whilst there is no equivalent recommended measure for adults, clinics can still model adult operational metrics on this NCQA recommendation.
3. ADHD patient outcomes
Untreated ADHD can have far-reaching consequences for patients and can impact school or work performance, social and family relationships, and make tasks requiring focus more difficult. These challenges can be difficult to measure quantifiably; however, for the patient, improvements in these areas can be life-changing.
Getting ADHD patients to set goals relating to their everyday quality of life and track progress against these goals is an important metric that is highly meaningful to both parties.
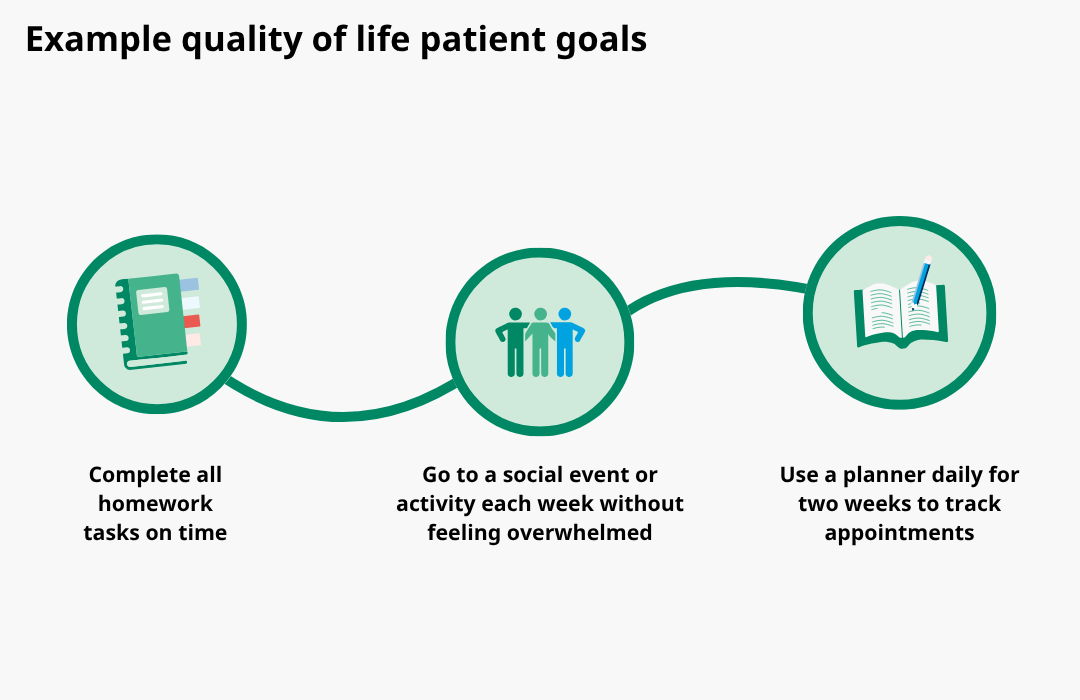
Disclaimer: These goals are included as illustrative examples and are not intended as medical advice.
The American Academy of Family Physicians recommends using the Adult ADHD Quality of Life Measure (AAQoL) questionnaire to track these improvements in daily life.
ADHD metrics: a 2025 checklist for clinicians
Achieving quality ADHD patient care is a product of improvements across three areas: clinical, operational, and patient outcomes. This checklist combines these metrics into a single list for clinical workflows.
Disclaimer: This checklist is for information only. It does not constitute medical or professional advice. Clinician discretion is advised.
Tips to add continuous improvement measures into an ADHD clinic
Clinicians are busy, and introducing metric reporting might feel like a challenge. However, here are some top tips for embedding performance improvement measures into ADHD care.
- Start small – introduce new reporting arrangements on a patient subset and take note of what works and doesn’t before attempting clinic-wide changes.
- Ensure ‘buy-in’ from clinicians, admin staff, and patients. Helping everyone to understand why tracking metrics is important will make it easier to adopt if it has support from all involved.
- Make use of existing tools and technologies. For example, the QbCheck output report presents patient data in an easy-to-interpret summary format and includes benchmarks.
- Use dashboards or report cards to visually present data and make reporting on these as part of clinic meetings/business planning.
Metrics as a driver of ADHD patient care improvements
Reporting ADHD metrics can help support improvements in patient care. As an example, some clinics trialed an ADHD internet portal where information such as rating scales could be inputted by parents, teachers, and pediatricians. Data was outputted in a report style for patient assessment. The study found that those clinics using the portal achieved more AAP-recommended ADHD care practices, such as the collection of rating scales, use of DSM-5 criteria, and using teacher rating scales to monitor treatment response.
ADHD metrics and the future of care
The use of metrics in ADHD care is a data-driven and technology-centric initiative. This represents a significant opportunity for clinics as health technology, data systems, and AI continue to improve and be adopted more widely.
Already, the Australian ADHD Professionals Association (AADPA) has launched an ADHD tracker that collects information from patients, parents, and teachers both in-clinic and between appointments. Data can be tracked over time, presented graphically, and shared with patients and family members.
Portals like this are likely to become more common as technology evolves. Patients may even prioritize clinics that use systems that can help them understand their condition more easily and that demonstrate a data-driven commitment to quality patient care.
Clinicians who capitalize on these opportunities now by adopting continuous improvement methods, introducing metrics, and incorporating data-driven objective technologies may find this positions them favorably to take advantage of future technologies and to be seen as a high-quality service provider by patients.