In ADHD care, where presentations vary, pathways can be complex, and demand continues to rise, consistency stands out as the defining trait of a successful, high-performing clinic. When patients receive the same standards of care with every clinician, at every appointment, success follows.
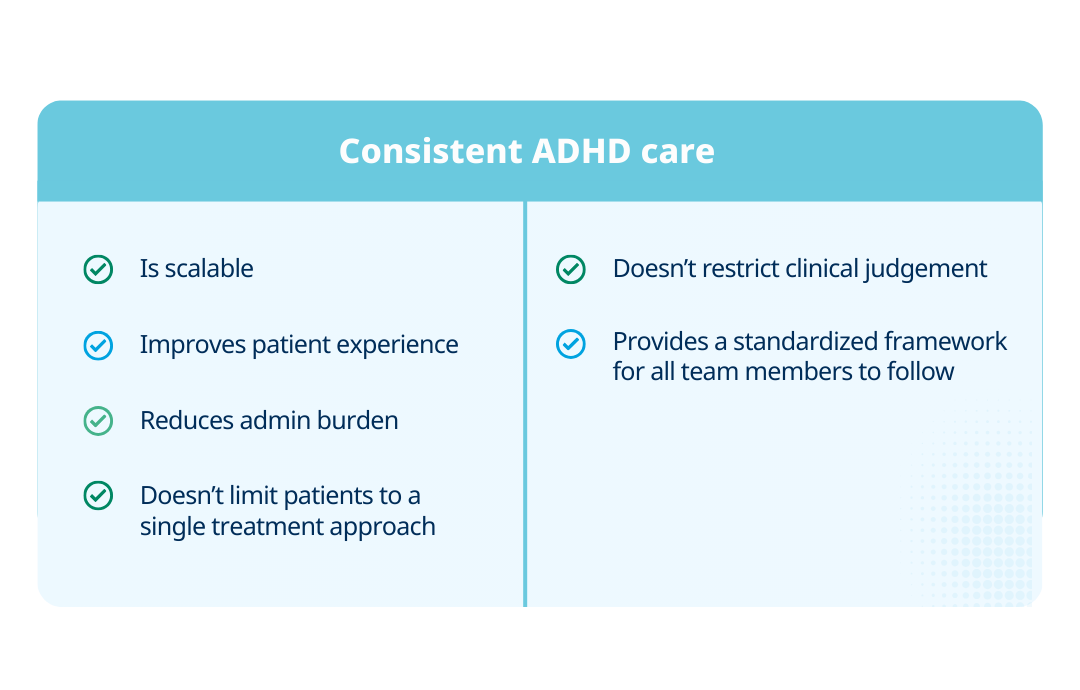
Developing a consistent model of ADHD care isn’t about trying to restrict clinicians or patients to following a one-size-fits-all pathway. It’s about establishing a scalable, standardized approach. In this blog, we look at what consistency really means and how it can support high-quality clinics to deliver a better patient experience.
What is the clinical impact of consistent ADHD care delivery?
ADHD affects patients of all ages and often requires treatment across the lifespan. Even adult diagnoses require evidence of symptom presence during childhood (before age 7 in DSM-IV, and updated to 12 in DSM-5). For clinicians, the availability of consistent, comparable data points throughout a patient’s life is key. It helps to track symptom change and treatment effect.
Through consistent ADHD care methods, you can safely diagnose, treat, and manage patients within a defined structure. Critical stages of the ADHD journey are established, repeatable, and scalable. This means using the same assessment tools, scheduling regular follow-ups, and consistently tracking symptom change. In short, consistency leads to better care, which improves overall patient outcomes.
How ADHD clinics can develop consistent models of care
Consistent models of care are built through structured pathways, standardized assessments, and shared systems that support operational efficiency and better patient outcomes. Here are some tips on how you can develop a successful model of care.
Develop shared data portals for optimal workflow
Shared digital portals can help ensure that data on ADHD symptoms, including rating scales and objective test results, is available and accessible to all clinicians treating a patient.
Clinics that integrate modern digital ADHD tests may have access to integrated data portals that facilitate the sharing of test results across multi-site clinic locations. They can also create patient profiles to keep all patient information together in a single location.
Design and implement a standardized and efficient patient pathway
A strong ADHD care pathway is evidence-based, repeatable, yet flexible enough to support patients’ personalized treatment plans. It reduces variation in assessment and treatment, improves safety, and ensures a clear, consistent patient experience.
The process of designing and developing a consistent pathway is iterative. The pathway goes through a process of continual improvement to arrive at the optimum solution. Patients benefit from this ongoing refinement through the removal of inefficiencies and duplicative processes.
The Dundee ADHD Clinical Care Pathway is a widely cited and replicated model demonstrating how effective pathway design supports consistent, quality ADHD care.
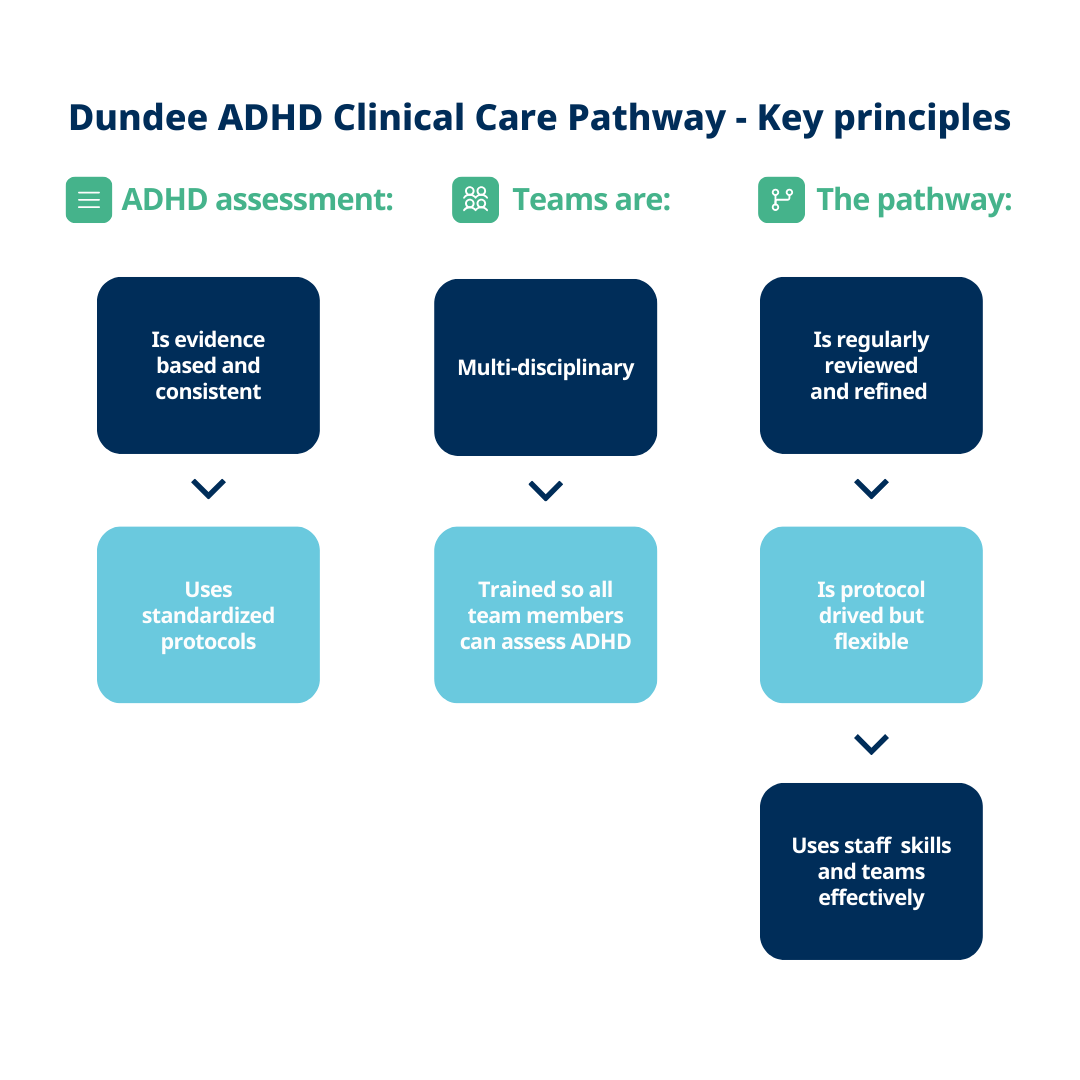
Infographic created based on the information from Coghill and Seth.
Use objective data to establish a consistent baseline for the patient population
Digital ADHD tests provide clinicians and patients with a quantitative baseline of ADHD symptoms. The test can be repeated at any interval, and results can be directly compared to see the impact of treatment. Even if a patient changes clinics or clinicians, they'll have a consistent measure of their ADHD symptoms over time.
Our practical benchmarking scorecard for ADHD clinics compares your practice to the standard so that you can keep providing modern, reliable ADHD care in 2026 and beyond.
How inconsistencies in care affect ADHD assessment and diagnosis
The AAP recommends diagnosing ADHD based on DSM-5 criteria, supported by rating scales to collect information from parents, teachers, and other sources. However, this is often inconsistently applied.
A recent study found 44% of clinicians did not ask about all 18 DSM-5 symptom criteria during ADHD testing. There was also a wide variation in which rating scales were used. 67.6% were using the Vanderbilt Assessment Scale, 54.1% Conners Rating Scales, and 16.2% the Child Behavior Checklist.
Despite the widespread use of rating scales, a systematic review concluded that no single assessment tool was adequate for ADHD diagnosis without additional testing methodologies.
Inconsistent approaches to ADHD assessment directly impact patient care and experience. Without a consistent baseline of symptoms, assessing treatment effect from medication becomes difficult. If a patient transitions between clinics, clinicians, or between primary and secondary care services, they are likely to end up being assessed on different criteria, exacerbating the problem.
How ADHD patients benefit from consistency
Building trust through care continuity
Continuity of care isn’t just about seeing the same healthcare professional. Standardized processes for diagnosis, treatment, and management can help build patient trust in their care. This continuity is especially important when patients may already feel uncertain or confused about their behaviors. Setting expectations and maintaining an open channel of communication shows reliability, which, over time, improves patient outcomes.
Legion Health, a Texas-based psychiatric clinic, introduced digital ADHD testing as a move to a more standardized and consistent model of ADHD care. Following standardization, time to diagnosis reduced and retention rates increased. There were also significant improvements in patient outcomes. Patients reported having an improved understanding of their symptoms, diagnosis, and treatment options.
How clinicians benefit from consistency
Scaling ADHD clinics and strengthening teams
For high-performing clinics, standardizing care can also provide a scalable model for expansion. Established processes can make taking on more patients easier, with reduced admin. Standardization also facilitates expansion to additional sites, as clinics have a ready-made roadmap for care they can implement.
Developing a consistent model of care also provides clinics with a defined product for marketing ADHD services to patients. Patients can be assured of a high-quality standard of care, whichever clinician they see, at any of the clinic’s locations.
Forming multidisciplinary teams (MDTs) is another recommended approach to evaluating ADHD. This not only aligns with NICE guidance but also offers real opportunities for improving care for patients and relieving pressure on clinicians’ workloads.
Adopting a standardized pathway, supported by informational continuity (shared electronic health records and clear communication protocols) can help address these concerns and support MDTs to operate effectively. Standardized processes also benefit the patient experience in MDT settings. Patients can be safely transferred between clinicians, and new patients can be efficiently onboarded to the pathway.
Looking ahead: structured care that adapts to a clinic’s needs
Recent trends in ADHD care point to the ADHD clinics of tomorrow being more data-led, scalable, and offering hybrid and virtual ADHD services. Developing a consistent pathway with standardized ADHD assessment and treatment processes supports clinics and patients and acts as a strong foundation for building future-ready ADHD clinics.
