Our understanding of ADHD, the symptoms, treatment options, and assessment methodologies, is evolving rapidly. In a short time, ADHD has gone from being considered a purely behavioral issue to being recognized as a complex neurodevelopmental condition.
Working in the field of ADHD means operating in an ever-evolving landscape. However, as our understanding grows, so do the opportunities for better identification of symptoms in different demographics, tailored treatments, and equitable care.
Latest research in ADHD treatment and medication
Identifying appropriate and effective treatments for ADHD is a critical concern for clinicians and patients. Continued research in this area can help clinicians make decisions supported by evidence and lead to more patients being placed on an effective treatment pathway.
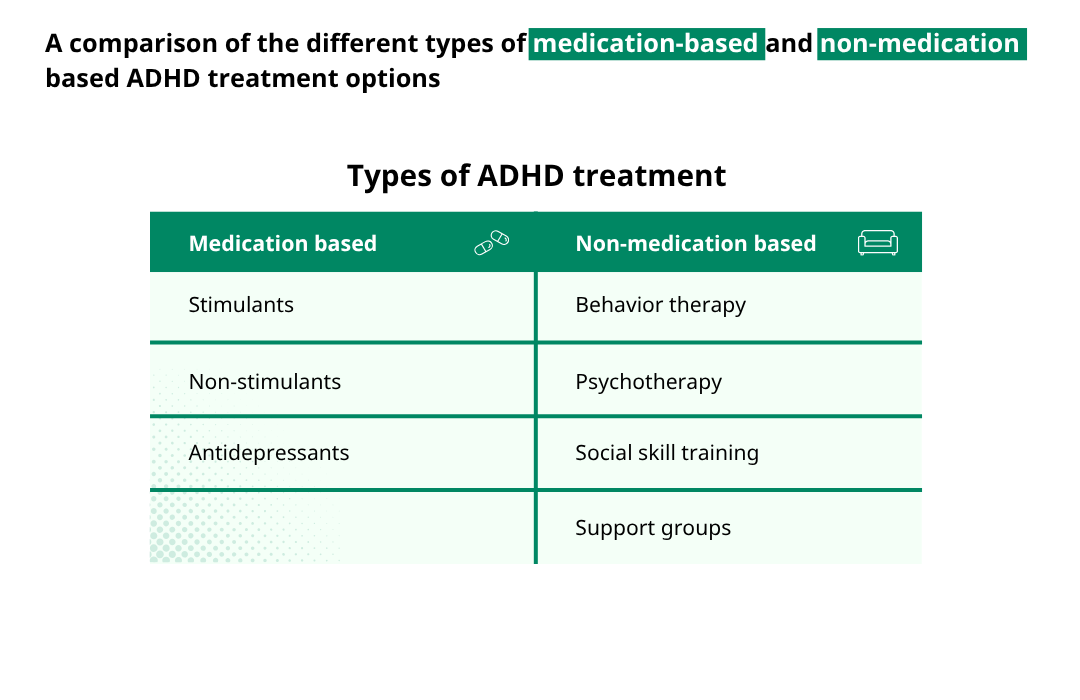
Published at the beginning of 2025, a major new study led by the University of Oxford and the University of Southampton investigated treatment effect on ADHD symptoms in adults after 12 weeks. They found that stimulants and atomoxetine were the only interventions with evidenced impact on reducing core ADHD symptoms in this period. The study did note, however, that there were tolerability and acceptability issues for patients associated with atomoxetine.
The study is significant for clinicians and could help support decisions over prescription advice. Stimulants have long been prescribed as an ADHD treatment, and the study by Ostinelli et al is a comprehensive assessment of the relative effectiveness of stimulants against other treatment types in a large patient sample group.
Two recent Swedish studies have also helped to quantify the impact of taking ADHD medications, like stimulants, on life expectancy and broader health. They support previous findings on the potential risks of untreated ADHD.
- Li et al., (2024) observed an 18.75% reduction in the overall risk of death in the two years after diagnosis for those taking ADHD medication.
- Taipale et al., (2024) found that taking ADHD medication helped to significantly lower a patient’s risk of suicidal behavior and hospitalization (for both psychiatric and non-psychiatric reasons).
Watch what happens if we do nothing about ADHD
New research into treatment effects is positive for clinicians and patients and shows the tangible benefits treatment can offer. It also evidences the need for ongoing research in the area, coupled with continuous education, and adding to published guidelines, to ensure that prescribing clinicians are aware of new developments.
Despite these encouraging findings, clinicians and patients continue to face challenges from ongoing medication shortages. CDC data from 2024 shows that 71.5% of US adults taking stimulant medication had difficulty filling their prescriptions in the previous year due to availability issues.
Further research identifying suitable medication alternatives and further action to minimize the impacts of shortages is crucial.
ADHD prevalence in 2025
Current data on the numbers or percentages of people diagnosed with ADHD is improving, and it is becoming easier to identify ADHD prevalence.
How many people have ADHD in 2025?
Recent data from the National Center for Health Statistics indicates that 15.5 million US adults had received an ADHD diagnosis by late 2023. Approximately 50% of these diagnoses were made in adulthood.
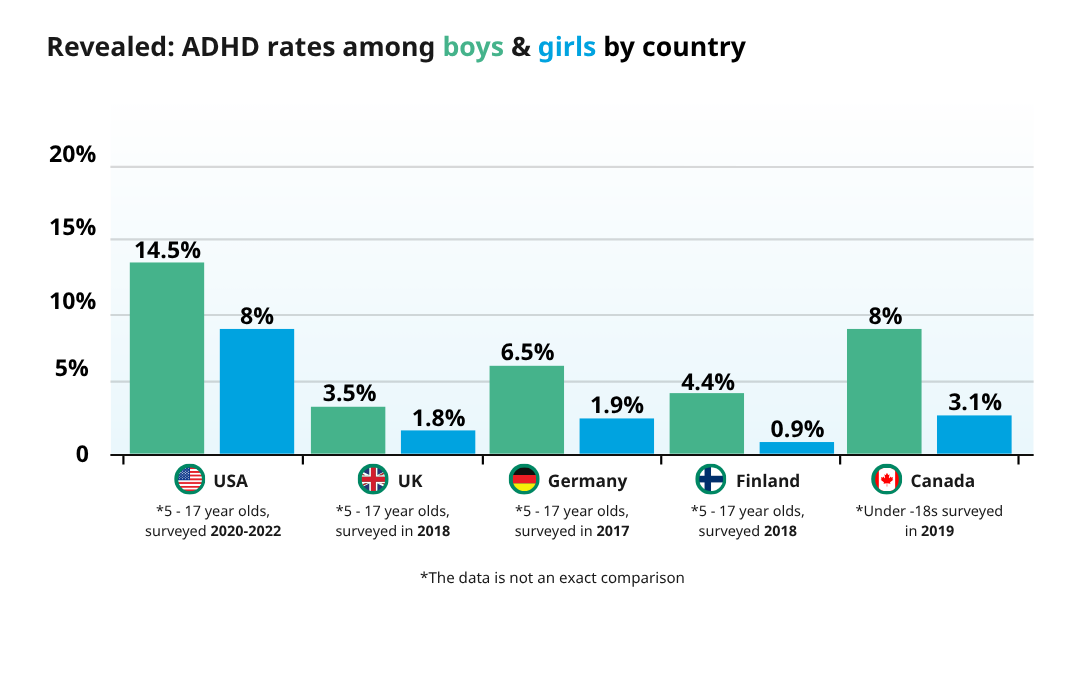
Additionally, a 2024 study reports that 7.1 million US children (around 11.4%) have received an ADHD diagnosis.
In the UK, the National Institute for Health and Care Excellence (NICE) estimates that around 5% of children and 3-4% of UK adults have ADHD.
ADHD was once thought of as a childhood condition, yet its prevalence and new diagnoses amongst adults demonstrates the lifelong nature of the condition. As more people become aware of symptoms, the identification of adults with ADHD is likely to continue.
How ADHD affects women and girls differently
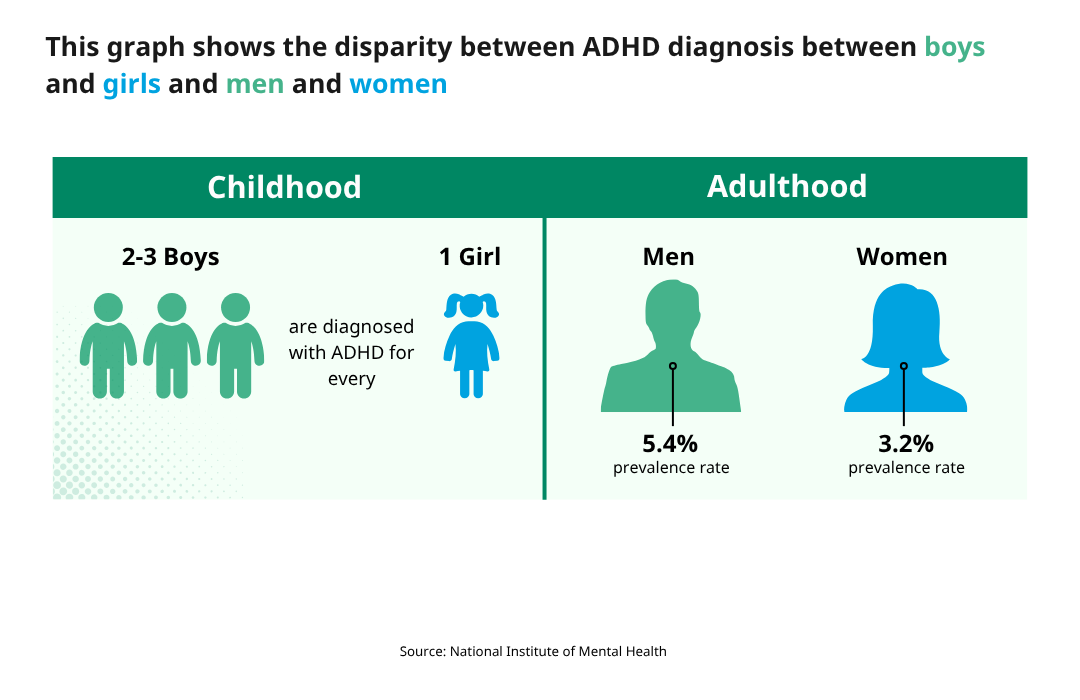
Our understanding of the different presentations of ADHD is continuing to develop. We know that women and girls are less likely to be diagnosed with ADHD than men and boys. We also know that female diagnoses often come later in life and that symptoms present differently in women and girls than men and boys.
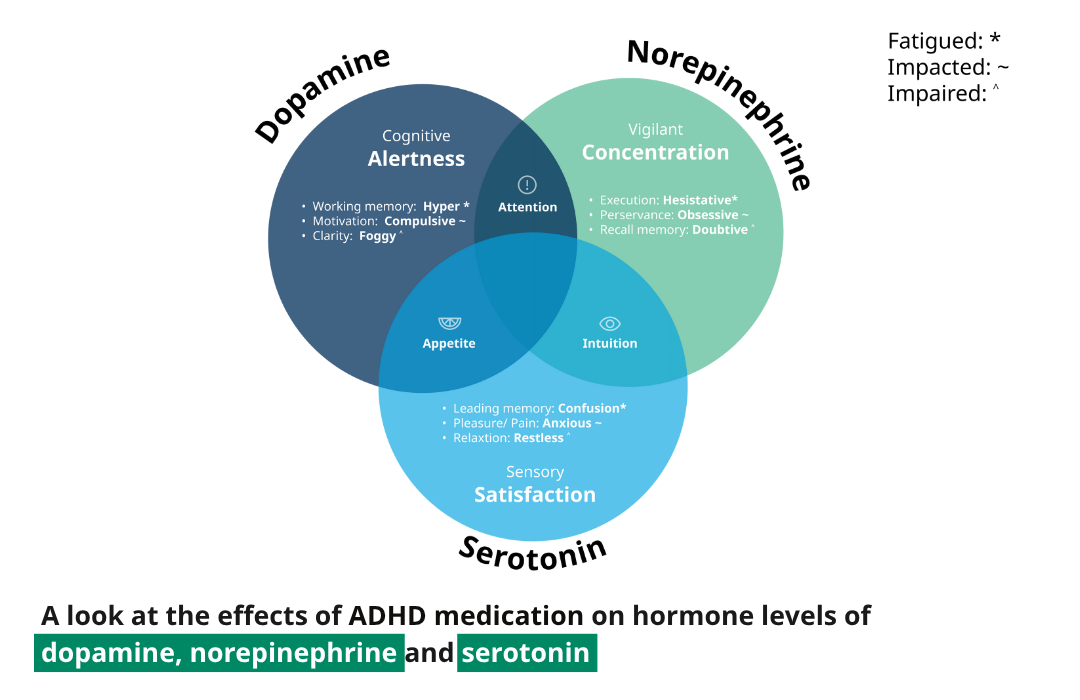
The relationship between changing hormone levels in females and ADHD symptoms is an evolving area of research. Clinicians assessing patients could find distinct differences in symptom presentation in women at different times in both their ovulatory cycle and lifespan. New research suggests that declines in estrogen levels can exacerbate ADHD symptoms, making symptoms more evident when estrogen is low e.g. during the early follicular phase (around the start of menstruation). Conversely, when estrogen levels are higher, ADHD symptoms may be less noticeable, e.g. during the late follicular phase just before ovulation, when estrogen peaks.
Clinicians may find that the timing of an ADHD assessment within a patient’s menstrual cycle can therefore have a bearing on symptom presentation. Repeat testing may be helpful and incorporating objective technologies into these evaluations could serve a valuable role by providing comparable data at recorded intervals.
Clinicians may also see more women presenting with ADHD as they move into perimenopause or menopause and estrogen levels decline. These women may not have previously noticed symptoms, making a later-life diagnosis more challenging. Objective measures help aid clinical decision-making in these complex cases where subjective assessments may be more difficult.
What guidance is available from national health organizations?
One of the challenges clinicians have faced historically when assessing patients for ADHD is the lack of overarching government guidance, however, this is now changing.
Later this year, the American Professional Society of ADHD and Related Disorders (APSARD) will publish guidelines for the diagnosis and treatment of ADHD in adults – a much-needed resource for clinicians.
In the UK, 2024 saw the publication of a significant new Diagnostic Guideline by the National Institute of Health and Care Excellence (NICE). The guidance provides clarity on ADHD assessment best practices by recommending the use of an objective test (QbTest) as part of the diagnostic process in children and young people aged 6-17.
Sweden’s National Board of Health and Welfare also published significant new guidelines on ADHD and autism in 2024.
Clinicians have a difficult role in assessing patients for ADHD and these guidelines provide critical advice. Such guidance also supports a more consistent approach to ADHD evaluation, which can help multi-site clinics in establishing standardized models of care.
ADHD assessments and the role of objective testing technologies
As more clinics incorporate objective ADHD testing technologies into pathways and research in the field continues to grow, we’re reaching new understandings of the application of the technology.
There is an established body of clinical research into the use of objective measures in ADHD evaluation and diagnosis. However, in 2024, two new studies highlighted the further usefulness of objective testing technologies for clinicians.
Sanyal et al., highlighted the potential use of objective tests like QbCheck, to aid treatment decisions, monitor the impact of ADHD medications on symptoms, and optimize treatments accordingly., monitor the impact of ADHD medications on symptoms, and optimize treatments accordingly.
Grossman and Berger suggest that the inclusion of a computerized test during assessment can increase patient trust in clinician decisions and also increase their intent to follow treatment recommendations.
A new era of awareness and acceptance of ADHD
Public awareness of ADHD is greater now than ever before. This new era of awareness has presented opportunities and challenges.
Social media has become a giant platform for discussion around ADHD. A 2025 study found that the top 100 #ADHD TikTok videos at the time of analysis had collectively been viewed nearly half a billion times. New content is posted daily, yet the study found fewer than 50% of the claims made in videos about ADHD symptoms aligned with the Diagnostic and Statistical Manual of Mental Disorders. This can present a serious challenge of misinformation, which is inevitably felt by clinicians receiving patients for assessment.
Other studies have highlighted this potential for social media-driven awareness to encourage more people to seek an ADHD diagnosis, placing further pressure on services that are already in high demand.
However, there are opportunities to be gained too. Greater public consciousness of ADHD can be a strong platform for lobbying. The ADHD Expert Consortium is one group driving change in the standard of ADHD care. As more clinical experts and patients join calls for action around ADHD, real change is possible.
What next for ADHD care?
Our understanding of ADHD continues to grow year-on-year. In a relatively short time, how we classify, assess, and treat ADHD has changed significantly. Availability of national guidelines, innovations in ADHD testing technologies, and expanding research on the effects of medication support clinicians in making difficult decisions when diagnosing ADHD.
Patients and patient welfare are at the heart of this drive to further our understanding of ADHD. Patients expect care that aligns with the emerging ‘Gold Standard in ADHD Care’. Meeting these high patient expectations is now the goal for healthcare providers, and new technologies, improved guidance, and streamlined care pathways can help with achieving this.