In 2025, the gold standard of ADHD diagnosis and treatment is evolving, shaped by updated DSM-5 criteria, new clinical tools, and a growing demand for timely, accurate care. Clinicians are facing rising ADHD prevalence, shifting diagnostic expectations, and increasing pressure to deliver structured, high-quality assessments.
But what defines gold-standard ADHD care today? Frameworks like those recommended by NICE in the UK offer one benchmark, but the principles of quality, accuracy, and efficiency apply globally. Across healthcare systems, the goal is the same: more accurate identification, more tailored treatment, and better outcomes for patients with ADHD.
In this guide, we’ll explore what high-quality ADHD care looks like in 2025 and beyond, drawing from the latest research, innovations in clinical tools, and practical frameworks designed to support clinicians every step of the way. Whether you’re reviewing your current diagnostic process or planning service improvements, this is your reference point for delivering ADHD care that’s not just compliant, but truly gold standard.
Understanding ADHD in 2025
Why is ADHD care evolving?
ADHD is no longer viewed as a condition limited to childhood, nor as one that follows a simple, linear path to diagnosis. In recent years, global awareness of ADHD has grown, alongside a sharp rise in adult ADHD diagnoses and increasing recognition of how the condition presents across genders and age groups.
Recent data shows ADHD prevalence is climbing worldwide, including in the UK, where referral rates have more than doubled in some regions. In the US, diagnoses among children and adolescents continue to trend upward. While this growing awareness is positive, it places added pressure on clinicians, not only to assess more individuals, but to do so with precision, speed, and fairness.
At the same time, expectations around ADHD care have changed. Today’s gold standard calls for structured, multi-informant evaluations, grounded in objective data and supported by scalable clinical frameworks.
The latest diagnostic frameworks
The foundations of ADHD diagnosis are shifting. With updates to both the DSM-5 and ICD-11, the criteria now reflect a broader, more inclusive understanding of how ADHD presents, particularly in adults, women, and neurodiverse populations.
In the DSM-5, changes include:
- Expanded symptom examples to capture adult experiences
- Emphasis on functional impairment across life domains
Meanwhile, ICD-11 introduces a more dimensional, transdiagnostic approach, aligning ADHD with other neurodevelopmental conditions and placing increased focus on clinical context.
For clinicians, this evolution means moving away from narrow symptom counts toward comprehensive, structured assessments, supported by multi-source data, validated tools, and clear clinical judgement.
Why this guide?
With so many variables at play, from evolving diagnostic frameworks to new digital tools and rising demand, clinicians need a clear, practical reference point.
This guide is designed to meet that need. Rooted in the latest research and clinical standards, it brings together everything you need to define and deliver gold-standard ADHD care in 2025 and beyond.
ADHD diagnosis – what does the future hold?
As the number of ADHD referrals continues to rise, especially in adult and female populations, the future of diagnosis depends on more than clinical instinct. Across health systems, clinicians are being asked to diagnose faster, more accurately, and more equitably, often with limited time and resources.
So, what does that future look like in practice? It means using digital tools that support structured decision-making. It means aligning with updated diagnostic criteria while reducing waitlists and variability. And it means building diagnostic workflow that reflect the realities of today’s ADHD presentations across ages, genders, and comorbidities.
Digital ADHD assessments in clinical use
Traditional diagnostic methods often rely heavily on subjective reports, making it difficult to distinguish ADHD from overlapping conditions. The shift toward digital ADHD assessments gives clinicians access to objective data that can complement clinical interviews and rating scales.
These tools don’t replace the clinician’s judgement, they enhance it. In 2025, digital assessments are increasingly being used to:
- Improve diagnostic accuracy
- Reduce reliance on single-source reports
- Support multidisciplinary team assessments
- Streamline processes for both adult and pediatric cases
"I’ve witnessed both under-diagnosis and over-diagnosis of ADHD. We absolutely need a more objective standardized approach. We cannot appropriately treat what we cannot see
- Theresa Cerulli, M.D.
Whether used in primary care, mental health services, or specialist clinics, objective tools are helping clinicians make clearer, faster decisions, especially when symptoms are complex or masked.
Designing diagnostic workflows for 2025
The rise in demand for ADHD assessments (particularly in adults) has put a spotlight on patient-journey design. In many settings, traditional approaches no longer scale. Clinics are turning to multidisciplinary teams, collaborative intake models, and structured protocols to manage increasing caseloads.
A future-ready clinical workflow might include:
- Screening and triage supported by digital tools
- Multi-informant interviews and rating scales
- Objective assessments integrated into the clinical workflow
- Collaborative input from psychiatry, psychology, and primary care
For clinicians, the goal is clarity: a clinical workflow that supports accurate identification without unnecessary delays.
What clinicians need in 2025
Looking ahead, the most effective ADHD diagnostic toolkits will be those that:
- Combine subjective and objective data
- Fit into existing clinical workflows
- Are validated across diverse populations
- Support evidence-based decision-making at every stage
Whether you’re reviewing your service model or exploring new technologies, now is the time to future-proof your diagnostic approach - for your patients, your team, and your outcomes.
ADHD treatment and medication titration
As ADHD diagnosis becomes more common across all age groups, the demand for effective, personalized treatment is rising. While stimulant medications remain the first-line treatment in many cases, the landscape is evolving, with greater emphasis on titration protocols, non-stimulant options, and a more nuanced approach to optimizing ADHD treatment plans.
For clinicians, the challenge is twofold: choosing the right medication and finding the right dose. This process needs to be quick enough to meet patient needs, while also being safe and precise to ensure long-term success.
Stimulant vs non-stimulant: A more individualized approach
In 2025, the most effective ADHD treatment will be tailored to the individual. While stimulants like methylphenidate and amphetamines are widely used due to their proven efficacy, not every patient responds the same, and not every case is straightforward.
Non-stimulant options, including atomoxetine, guanfacine, and newer extended-release formulations, are playing a larger role, especially for patients with anxiety, tics, or substance use concerns. The future of ADHD treatment is a more individualized toolkit: one that balances clinical guidelines with real-world complexity.
Best practices in ADHD medication titration (2025 and beyond)
Titration is a critical step in achieving treatment optimization, but it's also one of the most time-consuming and variable parts of the care journey. Inconsistent titration practices can lead to missed therapeutic windows, reduced adherence, and patient drop-off.
In 2025, best practice for titration includes:
- Clear dose escalation protocols based on age, comorbidities, and patient goals
- Ongoing monitoring of response and side effects (objective and subjective)
- Shared decision-making to support medication adherence
Clinicians are increasingly using technology-assisted monitoring tools and structured check-ins to reduce trial-and-error. Whether you’re working in a multidisciplinary team or private practice, having a clear titration workflow supports both clinical efficiency and patient confidence.
Common challenges and clinical considerations
Even with effective medications, treatment adherence can falter, especially if side effects aren't managed or expectations aren’t clearly set. Some common barriers clinicians report include:
- Poor communication around dosing timelines
- Overlooking sleep, appetite, or mood-related side effects
- Lack of engagement from patients or caregivers in follow-up
Addressing these challenges often comes down to proactive education, realistic goal setting, and building trust through transparent monitoring.
Multimodal treatment: beyond medication
While medication is often a first-line treatment for ADHD, it’s rarely the whole solution. In 2025, the gold standard in ADHD care is a multimodal approach, one that combines pharmacological treatment with behavioral therapies, environmental support, and coaching tailored to the patient’s needs.
While medication is often a first-line treatment for ADHD, it’s rarely the whole solution. In 2025, the gold standard in ADHD care is a multimodal approach, one that combines pharmacological treatment with behavioral therapies, environmental support, and coaching tailored to the patient’s needs.
Behavioral therapies and cognitive interventions
Evidence continues to support the use of CBT and behavioral interventions for patients with ADHD – especially when integrated with medication or used as standalone strategies for those who don’t choose pharmacological treatment.
What might these look like? In clinical settings, behavioral interventions may include:
- Cognitive behavioral therapy (CBT), including digital CBT tools
- Parent training programs (e.g. behavioral parent management training)
- Social skills training, especially in children and adolescents
These strategies help address executive functioning challenges, improve emotional regulation, and support treatment adherence over time. They're particularly valuable for patients with comorbid conditions such as anxiety or learning difficulties.
Lifestyle factors in ADHD management
Although not a replacement for clinical intervention, lifestyle factors such as sleep hygiene, structured routines, nutrition, and physical activity can play a key role in ADHD management.
Clinicians increasingly advise on:
- The impact of diet and exercise on cognitive performance and attention
- The role of sleep routines in improving daytime regulation
- Structuring environments to support task completion and reduce overstimulation
These recommendations are especially impactful when combined with clinical treatment plans and tailored coaching strategies.
"Visually seeing my individual symptom levels was particularly eye-opening. I wouldn’t have previously associated some of my behaviors with ADHD. And retesting (with QbCheck) let me see how medication was helping.”
Interventions at home and school
In pediatric cases, school-based interventions and caregiver strategies can be just as critical as in-clinic support. Clinicians working with children and families often coordinate across multidisciplinary teams to provide consistent, wraparound care.
Effective multimodal intervention plans may include:
- School accommodations (e.g. IEPs, 504 plans in the US)
- Regular communication with teachers and learning specialists
- Behavioral contracts or reinforcement systems at home
- ADHD coaching and support tools for caregivers
This integrated approach ensures that treatment doesn't just work in the clinic, but it works where it matters most: in real life.
Here's how educators can better support ADHD in the classroom: Download the toolkit
Defining quality ADHD care: success metrics
So, the important question: What does success look like in ADHD care?
It’s a question more clinicians are asking, not just at the point of diagnosis, but across the clinical workflow.
In 2025, the gold standard in ADHD services is outcome-driven: focused on measurable impact, not just process completion. From symptom improvement to functional gains, patient experience to adherence, quality ADHD care is now defined by data that reflects real-world results.
Common measures include:
- The Adult Self-Report Scale (ASRS) for tracking symptoms in adults
- The Vanderbilt Assessment Scale for children and adolescents / Conners-4
- Functional scales addressing attention, executive function, and emotional regulation
Clinicians are increasingly using these tools as part of structured treatment reviews, not just during diagnosis, but to track progress and guide ongoing care.
"As a practitioner and educator, I feel very strongly about using the latest technology to better serve both patients and future healthcare providers.
Using advances in objective testing for ADHD in conjunction with traditional subjective methods offers a more robust picture of a patient’s status, allowing providers to make a better diagnosis and giving patients clearer understanding of their health."
- Gary Kanter, MD, University of Florida
KPIs that matter: What clinics are measuring in 2025
More services are now building ADHD-specific key performance indicators (KPIs) to track and improve care delivery. These KPIs reflect both patient-facing outcomes and operational benchmarks.
Examples include:
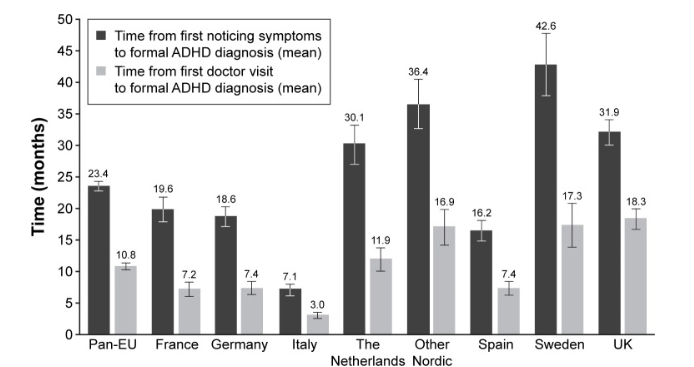
- Average time from referral to diagnosis
- Time to treatment initiation
- Percentage of patients with structured follow-up plans
- Symptom improvement at 3- and 6-month reviews
- Patient-reported outcome measures (PROMs)
These metrics help clinics assess what’s working, identify gaps, and support continuous service improvement.
"The time for change in behavioral health is not now, it was 20 years ago, and we missed it. We won’t stand by any longer.
The reality is that diagnosing ADHD is hard. With so many age-related and developmental questions at play in competition with our own biases, nothing is more important to the future of ADHD diagnosis than the widespread adoption of objective testing measures."
- Evelyn Polk-Green, Educator and Past President ADDA and CHADD
Patient satisfaction and engagement
Success in ADHD care isn’t only about clinical data, it’s also about how patients and families feel during the process. Are they supported? Heard? Confident in their care plan?
Measuring satisfaction and engagement is increasingly viewed as essential to high-quality ADHD services, especially in multidisciplinary settings. This may include:
- Feedback surveys post-diagnosis or during titration
- Goal-setting sessions with patients and families
- Engagement metrics like follow-up attendance and medication adherence
Data-led decision making in everyday practice
Ultimately, delivering quality ADHD care in 2025 means using data to inform clinical decisions, not to replace them.
Whether you’re reviewing a treatment plan, managing a complex case, or refining your service model, access to consistent, meaningful data allows you to provide care that’s not just effective, but accountable.
Measuring long-term success in ADHD care
Three months after diagnosis, a patient stops attending follow-ups. Their symptoms haven’t worsened, but they haven’t improved either. No changes have been made to their medication.
For clinicians, this kind of dropout isn’t rare. But it is a missed opportunity… for progress, for engagement, for real, lasting care.
In 2025, quality ADHD services are looking beyond short-term symptom relief. They’re asking a harder question: What does success look like long-term?
Challenge 1: tracking outcomes beyond the first prescription
Clinical success doesn't end at titration. To deliver long-term value, services must monitor sustained outcomes - functional gains, medication adherence, and emotional wellbeing.
What long-term tracking looks like in practice:
- Scheduled check-ins at three, six, and 12 months
- Use of follow-up tools like QbCheck or, the ASRS or Vanderbilt Assessment Scale
- Medication reviews with dose adjustments based on lived experience
- New goals and interventions as life changes (e.g., school transitions, job stress, parenting)
Long-term care is dynamic. Progress isn't linear. The best ADHD clinics are designing follow-up strategies that reflect that.
Challenge 2: closing the retention gap
Clinicians know the pattern well: initial engagement is strong, titration is complete, but somewhere between the three and six-month mark, the patient fades out of view. No major red flags, just a quiet drift. Appointments rescheduled, then missed. Prescriptions left unfilled. Progress, paused.
For adolescents, it’s often school pressures or social stigma. For adults, it might be job demands, caregiving responsibilities, or simply the emotional fatigue of managing a new diagnosis. Regardless of the reason, the outcome is the same, disengagement, and with it, a return of unmanaged symptoms.
Retention isn’t just about logistics. It’s about building care plans that feel sustainable, not overwhelming. It’s about ensuring patients see the value of staying connected, even when things are going well.
Clinics addressing this gap are shifting their mindset. They’re moving away from reactive follow-ups and toward proactive relationship-building. This includes everything from telehealth flexibility and patient-led goal tracking to scheduled check-ins that aren’t just administrative, they’re supportive, meaningful, and expected.
Technology and innovation in ADHD care
“Digital tools aren’t replacing clinical decisions – they’re enhancing them.”
That’s the mindset guiding many of the most forward-thinking ADHD clinics in 2025. Technology isn’t a gimmick, it’s a response to real pressures: long waitlists, diagnostic inconsistency, and the demand for clearer, faster decisions.
Whether you're navigating a complex case or simply aiming to streamline assessments, digital health innovations are no longer optional, they’re essential.
AI in ADHD: cutting through the noise
There's plenty of hype about AI, but what’s actually useful in ADHD care today?
Clinically relevant AI tools in 2025:
- Pattern recognition across large patient datasets
- Risk modelling for dropout or non-response
- Intake triage support using NLP-based patient summaries
- Adaptive treatment planning based on real-time outcomes
What clinicians need isn’t automation – it’s augmentation. Tools that surface meaningful insights, without removing professional judgement.
Spotlight: objective data in practice
Let’s say a patient presents with inattention, but it's unclear whether it’s ADHD, anxiety, or sleep related. Behavioral history is mixed. The school report conflicts with the parent rating scale.
In this scenario, a computer-based ADHD assessment that delivers objective, quantifiable data, like QbCheck, becomes a decision-making asset. It helps confirm or rule out core ADHD symptom patterns and brings a layer of clarity to complex presentations.
Objective tools aren't a shortcut, they’re a second set of eyes. And in busy clinical settings, that clarity matters.
Integrating tech without overwhelm
No clinician needs another login, another platform, or another checkbox.
The most effective clinics are:
- Embedding digital assessments directly into patient flow
- Training teams to interpret and communicate results clearly
- Using telehealth ready platforms that support consistency across remote and in-person settings
- Tracking digital engagement (e.g. coaching apps, reminders) as part of treatment adherence
When well-integrated, tech doesn’t disrupt care, it deepens it.