ADHD is a complex condition, and patients often have comorbid conditions such as autism or anxiety. This can make diagnosing ADHD difficult, especially in primary care settings. One response to this challenge in the UK has been the establishment of multi-disciplinary teams (MDTs). These team structures mean that patients can be seen by specialists earlier in the care pathway and receive a diagnosis quicker.
What are multi-disciplinary ADHD teams?
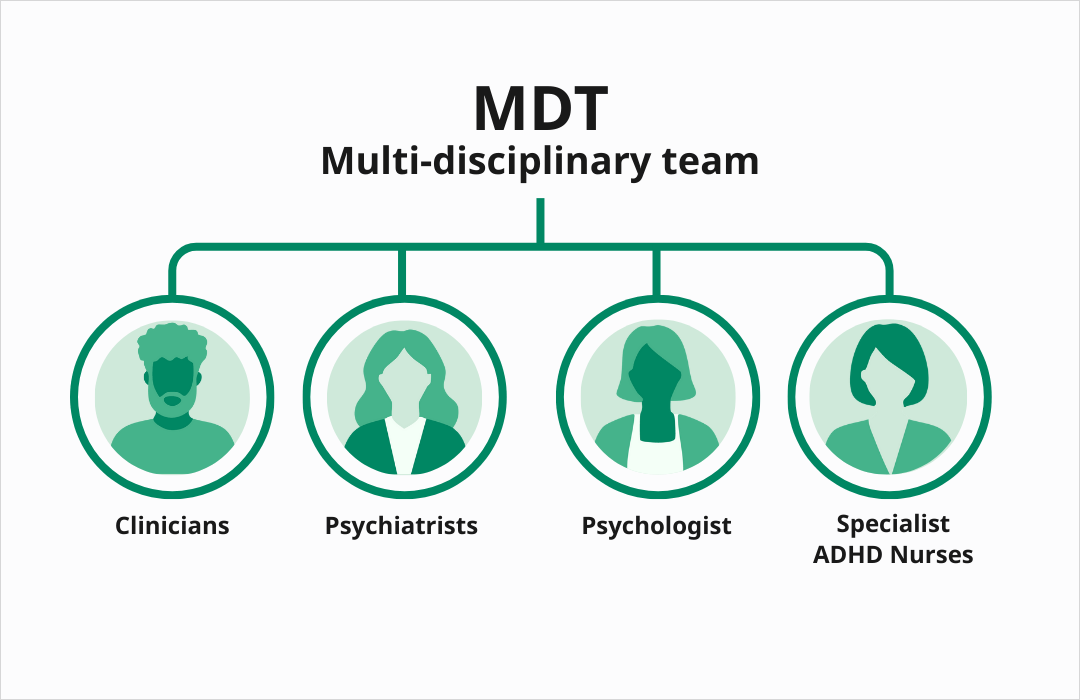
A multi-disciplinary team (MDT) is made up of medical professionals from different specialisms. This may include GPs or clinicians, psychiatrists, psychologists, and specialist ADHD nurses. For diagnosing child ADHD, education specialists, social workers, and teachers may also work closely with the team.
NICE recommends multi-disciplinary teams for ADHD care in the UK
The National Institute for Health and Care Excellence (NICE) recommends a multi-disciplinary approach to ADHD care in NG87:
“Mental health services for children, young people and adults, and child health services, should form multidisciplinary specialist ADHD teams”
ADHD metrics: a 2025 checklist for clinicians
Achieving quality ADHD patient care is a product of improvements across three areas: clinical, operational, and patient outcomes. This checklist combines these metrics into a single list for clinical workflows.
Disclaimer: This checklist is for information only. It does not constitute medical or professional advice. Clinician discretion is advised.
What are the benefits of a multi-disciplinary team approach?
Given the challenges in diagnosing ADHD, could MDTs help to improve patient care and streamline pathways for clinicians? Let's find out.
Help identify comorbidities
ADHD symptoms can be masked by the presence of comorbid conditions. A multi-disciplinary approach to diagnosis means that a patient can be seen by experienced specialists, including psychiatrists, psychologists, and ADHD nurses who can work together to undertake a comprehensive assessment, identifying both ADHD and comorbid conditions.
Reduce wait times for ADHD assessment
One of the strengths of MDTs is that they can work more flexibly. Bullock and Ford share how establishing a nurse-led MDT team in North Staffordshire facilitated a reduction in ADHD wait lists.
The MDT included nursing leads, psychiatrists, psychologists, parenting and play specialists, and healthcare support workers. The nursing leads utilized objective testing to assess patients for ADHD (alongside subjective measures), enabling them to complete assessments promptly and with increased confidence.
90% of patients in the area’s ADHD teams are now seen under this shared-care approach. This has relieved pressure on the psychiatry team members, with nurse practitioners taking on more of the work. The study estimated a saving of £202,000 a year in prescription costs and a reduction in referral-to-outcome times from 18-24 months to 0-12 weeks.
Support for the transition from child to adult ADHD services
The CATCh-uS study found that fewer than a quarter of ADHD patients successfully make the transition from child to adult ADHD services in the UK.
In NG87, NICE highlights the need for MDTs to establish communication and information-sharing protocols between pediatric, child and adolescent, and adult mental health services. They specifically reference transition arrangements between child and adult services.
These strengthened communication protocols mean that patients engaging with MDTs have greater opportunities for continuity of care and for receiving ADHD treatment into adulthood.
A multi-disciplinary approach to ADHD treatment
There is evidence to suggest that multi-disciplinary responses to ADHD can benefit patients in treatment as well as diagnosis.
A 2023 study into the treatment of ADHD in children highlighted the effectiveness of combination treatments delivered by a multi-disciplinary team. They found that a combination of medication, parent training, cognitive behavioral therapy, sensory integration training, and sand tray therapy resulted in a treatment efficacy of 91.84%, compared with 75.51% for treatment alone.

What clinicians need to consider when establishing multi-disciplinary teams
Setting up a multi-disciplinary team may mean a significant change to existing ADHD care pathways and new challenges for clinicians.
The role of care coordinators within multi-disciplinary ADHD teams
Patients engaging with multi-disciplinary teams may see several different healthcare professionals during their diagnosis and treatment. Instating a care coordinator role within an MDT can help to avoid any gaps in service provision. Care coordinators are important contact points for patients, family, and carers, and act as a bridge between service providers.

Multi-disciplinary teams: The standard for ADHD care in the UK?
It’s been over seven years since the publication of NG87 and NICE’s recommendation that multi-disciplinary teams be formed for ADHD diagnosis and care in the UK.
However, adoption of the MDT approach has been inconsistent geographically and many UK patients still face challenges in receiving a timely ADHD assessment. A 2022 report by the Centre for Mental Health outlined that at their least effective, UK mental health services could be ‘fragmented’ and late in their interventions.
Establishing multi-disciplinary teams not only aligns with NICE guidance but it offers real opportunities for improving care for patients and relieving pressure on clinicians’ workloads. The challenge UK clinicians now face is to facilitate the more widespread adoption of the MDT model.
