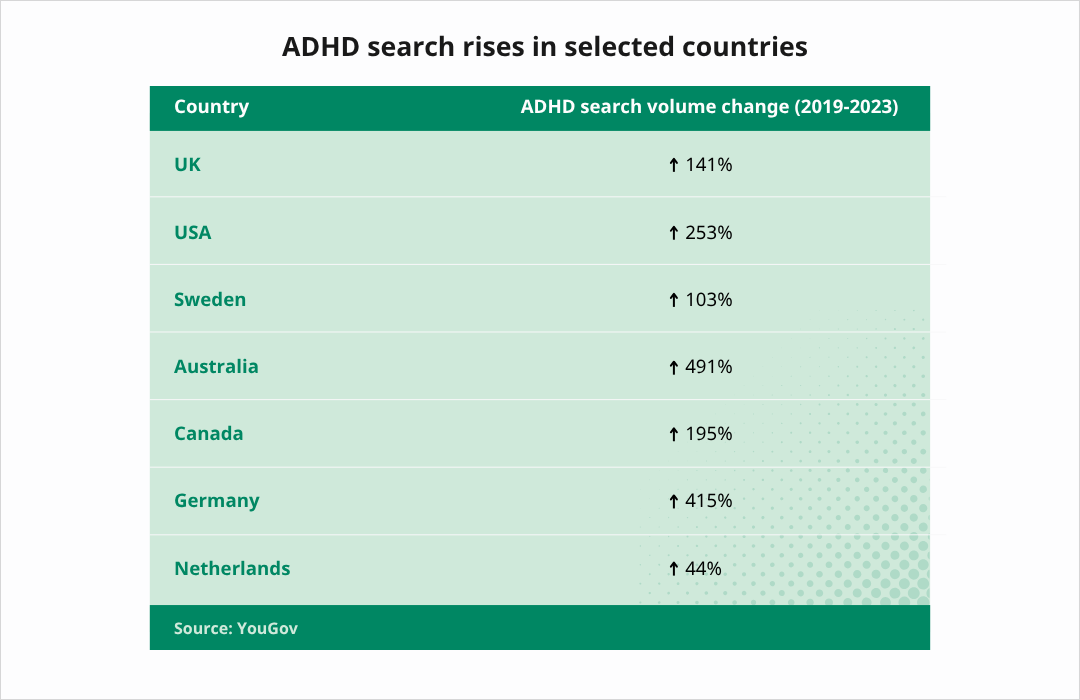
There’s been a noticeable rise in media and public interest in ADHD in recent years. A 2024 YouGov study found that online searches for the term “ADHD” increased significantly in 19 out of 20 countries between 2019 and 2023, with an average percentage increase of +270.5%.
One question remains, are ADHD rates increasing or is it simply that awareness and interest in the condition has grown? We take a look at the data and consider the factors that may fuel an increase in ADHD diagnoses.
Continued impact from the pandemic
The COVID-19 pandemic catalyzed the adoption of telehealth services, particularly for mental health care. Virtual providers have since become critical in meeting this growing demand:
- Behavioral health telehealth utilization: Telehealth visits for behavioral health grew from 41% in Q1 2020 to 67% by Q3 2023.
- Medicare telehealth adoption: A 63-fold increase in Medicare telehealth usage was reported during the pandemic, with behavioral health services leading the way.
- Sustained growth: Telehealth utilization remains above pre-pandemic levels, with patients increasingly preferring the convenience and flexibility it offers.

Is there a rise in ADHD diagnoses?
There is evidence to suggest that the rate at which people are diagnosed with ADHD is increasing.
Danielson et al., report that approximately 1 million more US children had been diagnosed with ADHD in 2022 compared with 2016. Meanwhile, a UK study analyzing data from 2000 to 2018 saw a twenty-fold increase in adult ADHD diagnoses across the period.
ADHD prevalence has increased in the US this past decade. In 2000, around 6-10% of US children were estimated to have ADHD Danielson et al. report that by 2018, some estimates have risen to 9-10%.
What's causing a rise in ADHD diagnosis?
It’s important to highlight that our understanding of ADHD in 2025 is so much more advanced than when the earlier data points were taken. How we classify and diagnose ADHD has changed, as well as our understanding of symptom presentation in different people. These factors can all help to explain the statistics behind ADHD growth.
Increased awareness among physicians, particularly in underrepresented minorities and women
In a relatively short time, ADHD has gone from being thought of as a childhood condition that mainly affects boys to a nuanced lifelong condition with complex presentations. Clinicians are seeing more adult ADHD patients and this recognition that ADHD affects adults as well as children has been linked to the increase in adult ADHD diagnoses.
Research and symptom criteria are also being expanded to recognize that symptoms may present differently for women and minorities. Often these individuals may have been living with ADHD for many years before a diagnosis is made.
The evolution of the diagnostic criteria accounts for some of the rise in ADHD
The DSM-5 is a critical manual for clinicians assessing patients for neurological conditions. In 2022 the symptom criteria for diagnosing ADHD were expanded with additional commentary on how symptoms may present for adults. This change facilitates the diagnosis of more adults with the condition and highlights the increased demand for adult ADHD symptom criteria.
ADHD has also become prominent in pop culture
ADHD has become more visible. Regular news coverage, social media discussions, celebrities sharing diagnoses, and popular culture storylines have all helped to raise awareness of the condition and symptoms.
Social media and its role in ADHD awareness
The internet, and specifically social media, has made information on ADHD widely accessible and sharable. A study published earlier this year analyzed the top 100 videos on TikTok using #ADHD. Collectively, they had been viewed nearly half a billion times.
Benefits to clinicians and ADHD awareness
Social media has met some of the demand for information in traditionally underrepresented demographics. For instance, how ADHD symptoms affect women has historically been underreported, with the majority of research focusing on men and boys. Yet as much as 62% of online ADHD discussion is by female users.
Increased visibility of ADHD online and in public consciousness can have its benefits. These online discussions can help destigmatize the condition and make conversations with friends, family, and healthcare professionals more accessible.
Recent progress around governments announcing or publishing new ADHD guidance, may also be partly down to this increased awareness and attention.
Online misinformation and negative impacts on clinicians
A major downside of social media is the spread of misinformation on ADHD. That same analysis of the top 100 TikTok videos found that fewer than 50% of the claims around ADHD symptoms aligned with the DSM-5 criteria.
Social media misinformation and self-diagnoses are also placing increased pressure on clinics. As an example, Seattle-based psychologist Sophia Rath said in 2023 that TikTok “drives at least 50% of our current requests for intakes”.
Are ADHD rates increasing or are diagnoses just “catching up”?
These issues of the late recognition of adult ADHD and reduced awareness of female symptoms have likely led to ADHD being underdiagnosed in the past. Abdelnour et al. suggest this remains an ongoing problem. They highlight that recent studies continue to show Black Indigenous and Persons of Color (BIPOC) and females being underdiagnosed or diagnosed later in life. So, the current increase in ADHD diagnoses could be a result of people whose ADHD symptoms have previously been missed, finally coming forward for assessment.
What next? Will ADHD diagnostic rates continue to climb?
Clinicians will likely continue to face high demand for ADHD assessment from people with undiagnosed ADHD as the historic underdiagnosis of the condition levels out. However, there will come a point where diagnosis catches up with prevalence. At this stage, referrals should stabilize and pressure on clinics will reduce. Importantly for patients, this will mean that undiagnosed cases of ADHD become increasingly rare and more patients will get the support and treatment they need.
